In the paradigm of science-based medicine, ideally basic science discoveries are translated into human treatments in a multistep process involves discovering a mechanism, testing that mechanism in cell culture and animals, and then introducing a treatment based on that biological mechanism into human patients by testing it in a series of increasingly rigorous clinical trials that culminate in large phase III randomized controlled efficacy/safety trials. Of course, science can be messy, and it’s often more complicated than that, with the various steps being carried out in orders different than what I describe, or simultaneously, or sometimes missing a step. Then, of course, after testing in humans, additional observations are made, taken back to the laboratory, and the whole process can start again in order to try to refine and improve the treatment discovered. For treatments whose prior plausibility has been demonstrated in preclinical experiments, though, the randomized, double-blind controlled clinical trial remains the final arbiter if a treatment “works”. The ethics of these trials usually demands, with rare exceptions, that the patients agreeing to be human subjects in the trial be free of incentive or coercion, which usually means that they should not pay to be a part of the trial; the sponsor, the company or investigator testing the new treatment, pays. In the past, I’ve been very critical of people and companies undertaking “pay-to-play” clinical trials, such as Stanislaw Burzynski and various dubious stem cell clinics that have at times managed to turn the US database of clinical trials, ClinicalTrials.gov, into a marketing tool for their scientifically worthless pay-to-play uncontrolled observational trials. Never, however, have I seen anything like what Libella Gene Therapeutics, LLC is doing, which I learned about right before the holiday break here in the US:
"Libella's clinical trial has been posted at the United States National Library of Medicine (NLM)'s https://t.co/7VDbgFpTJL database." $1 million a person for this "pay-to-play" study and of course it makes it into ClinicalTrials dot gov. https://t.co/ZmgYVYzLoq
— Leigh Turner (@LeighGTurner) November 25, 2019
And:
"This is the world's first IRB-approved clinical trial aimed at reversing aging by at least 20 years; it is also the world's most expensive pay-to-play trial with a one million price tag to enroll." The fee is $1 million per person. 💰💰💰 https://t.co/ZmgYVYzLoq
— Leigh Turner (@LeighGTurner) November 25, 2019
And:
Telomerase gene therapy in mice delays aging and increases longevity. https://t.co/Nh54LHVdcH <- World's most expensive pay-to-play trial.
Libella's clinical trial involves a new gene-therapy using a proprietary AAV Reverse Transcriptase enzyme & aims to lengthen telomeres.
— Comprehensive Cell Solutions @CCS_NYBC (@CcsNybc) November 26, 2019
I had thought that Burzynski and the various quack stem cell clinics I’ve come across over the years requiring participants in their “clinical trials” to pay to be in them were bad, but Libella Therapeutics takes the abuse of the clinical trial process to a whole new level, and it’s not just because of the eye-popping price tag, which is more than three times higher than any previous pay-to-pay price tag that I’ve ever seen before. Let’s first take a look at the press release, and then I’ll describe what I discovered doing a bit more digging.
The hype: A “breakthrough” anti-aging treatment
When I first saw the Tweets about Libella Gene Therapeutics’ press release last Monday (the date of the press release was November 21), I was debating whether to write about it right away (before the Thanksgiving holiday) on my not-so-secret other (and pseudonymous) blog, but I decided that this was more appropriate as SBM material and could wait. So I waited a week. In the interim, I was disappointed to see very little published about it, other than promotional articles and some criticism on Twitter by Leigh Turner and some others.
So let’s go to the press release. Let’s see what Libella has to say about it:
Libella Gene Therapeutics, LLC (“Libella”) announces an institutional review board (IRB)-approved pay-to-play clinical trial in Colombia (South America) using gene therapy that aims to treat and ultimately cure aging. This could lead to Libella offering the world’s only treatment to cure and reverse aging by 20 years.
Under Libella’s pay-to-play model, trial participants will be enrolled in their country of origin after paying $1 million. Participants will travel to Colombia to sign their informed consent and to receive the Libella gene therapy under a strictly controlled hospital environment.
Traditionally, aging has been viewed as a natural process. This view has shifted, and now scientists believe that aging should be seen as a disease. The research in this field has led to the belief that the kingpin of aging in humans is the shortening of our telomeres.
No red flags there, right? I mean, seriously. This trial has more warning signs of being a scam than any I’ve seen in a really long time. Sign the patients up in their own country? Require them to pay $1 million up front before enrollment and travel to Columbia for treatment? Make them pay up before signing informed consent? (If the patient changes his mind between signing up in his home country and signing informed consent in Colombia, can he get his money back?) Why on earth did the company choose this method, instead of going for FDA approval, and doing it the right way? Obviously, Libella Gene Therapeutics must be sensitive to the criticism of profiteering, because the press release includes this rather unconvincing explanation:
On why they decided to conduct its project outside the United States, Libella’s President, Dr. Jeff Mathis, said, “Traditional clinical trials in the U.S. can take years and millions, or even billions, of dollars. The research and techniques that have been proven to work are ready now. We believe we have the scientist, the technology, the physicians, and the lab partners that are necessary to get this trial done faster and at a lower cost in Colombia.”
I would counter that, more than anything else, it sounds more like their wanting to transfer development costs to the patient in order to profit. That’s my opinion, and I’m not alone, obviously. Moreover, as you will see, the principal investigator in Colombia and the facility where the trial will be carried out does not inspire confidence.
What, specifically, is the treatment that Libella is testing? According to the press release:
Telomeres are the body’s biological clock. Every time a cell divides, telomeres shorten, and our cells become less efficient at dividing again. This is why we age. A significant number of scientific peer-reviewed studies have confirmed this. Some of these studies have shown actual age reversal in every way imaginable simply by lengthening telomeres.
Bill Andrews, Ph.D., Libella’s Chief Scientific Officer, has developed a gene therapy that aims to lengthen telomeres. Dr. Andrew’s gene therapy delivery system has been demonstrated as safe with minimal adverse reactions in about 200 clinical trials. Dr. Andrews led the research at Geron Corporation over 20 years ago that initially discovered human telomerase and was part of the team that led the initial experiments related to telomerase induction and cancer.
Telomerase gene therapy in mice delays aging and increases longevity. Libella’s clinical trial involves a new gene-therapy using a proprietary AAV Reverse (hTERT) Transcriptase enzyme and aims to lengthen telomeres. Libella believes that lengthening telomeres is the key to treating and possibly curing aging.
Before we proceed, I’ll indulge in a little basic science. A telomere is a stretch of repetitive nucleotide sequences at each end of a chromosome. For the basics about telomeres for people not trained in molecular biology, the Wikipedia entry is a quite acceptable entry point. The basic concept is that, due to how DNA is replicated, the enzymes that duplicate DNA can’t duplicate it all the way to the very end of the strand. Each cell division, each duplication, of a chromosome, therefore results in loss of nucleotides at the end of the chromosome and thus some shortening of the chromosome. In some cells, to counter that, there’s an enzyme, telomerase reverse transcriptase (often just called telomerase or abbreviated as TERT or hTERT), that replenishes telomeres, adding the aforementioned repetitive sequences to the ends of the chromosomes.
So why do we age? One mechanism behind aging is the telomere. Telomerase is not made in all (or even in most) cells. Thus, in differentiated cells each telomere becomes shorter, and this is indeed thought to play a role in aging, with deficiencies in telomerase activity are associated with aging and genetic syndromes, such as cri du chat. There are exceptions, of course. For instance, telomerase is made in stem cells and certain reproductive cells and responsible for their ability to continue to replicate nearly indefinitely. Not surprisingly, given its function in preventing senescence (the loss of the ability of a cell to replicate that can occur when telomeres become too short), making too much telomerase is associated with cancer, although telomerase alone doesn’t appear to cause cancer (more on that below).
To boil that passage all down, what Libella is proposing to do is to use AAV (adeno-associated virus) as its vector to deliver the gene for hTERT to cells. AAV is a common vector used to introduce coding sequences for genes into cells and has many attractive features for use in gene therapy, including lack of pathogenicity, ability to infect both dividing and non-dividing cells, and ability to stably integrate into the host cell’s genome at a specific site on human chromosome 19. There have been a number of clinical trials of gene therapy using AAV as the delivery vector for the therapeutic gene. Indeed, the first gene therapy product to be approved by the FDA is an AAV-based therapy, LUXTURNA™ (voretigene neparvovec-rzyl; Spark Therapeutics, Inc., Philadelphia, PA), which delivers a normal copy of the RPE65 gene to retinal cells for the treatment of RPE65 mutation–associated retinal dystrophy, a disease that results in blindness. The main downsides of AAV for delivering gene therapy are that it doesn’t have the packaging capacity to deliver large genes and, because it’s a virus, it can provoke an immune response, leading to resistance as the body eliminates the virus.
Right off the bat, one can see that, depending upon the preclinical data developed by Libella, the idea that telomerase treatment could impact human aging is not entirely implausible. The marketing materials do, however, go beyond simplified into the realm of simplistic. Aging is not as simple as the company’s promotional materials make it sound. Let’s take a look at a booklet included with the press release, Bill Andrews on Telomere Basics: Curing Aging.
Does bad graphics mean bad science?
The first image in the booklet is an atrocity against graphics that looks as though someone made it on an animation application from 15-20 years ago:
One might accuse me of being petty, but one would think that someone like Bill Andrews could afford to hire a more competent graphic designer. Obviously, bad graphics don’t necessarily mean bad science, although the opening passage does not give me confidence, in particular his emphasis of the claim made in the press release that aging is a disease:
But, in some multicellular organisms, such as humans, certain cells strayed from the germ line and began to exhibit signs of aging. These cells aged because they became afflicted with a disease: their ability to reproduce themselves indefinitely became broken. The cause of this disease is still speculative, but many scientists are searching for cures.
The fact that a disease has existed in the genetic code of an animal for a very long time does not mean that it is not a disease. Thousands of diseases, from hemophilia to cystic fibrosis, have lurked in our genes for far longer than recorded history. These diseases should be cured, and aging is no exception.
Yes, but neither hemophilia nor cystic fibrosis nor all those other genetic diseases affect each and every living sexually reproducing multicellular organism with, proportionally speaking, few exceptions, nor have they affected each and every such organism since multicellular organisms first started to evolve billions of years ago. To simplify (but hopefully not to oversimplify), there’s a tradeoff between becoming multicellular and having cells that can reproduce indefinitely, the former requiring the controls on cell duplication and cells that eventually undergo senescence and the former being a risk for uncontrolled replication, one form of which is cancer. In any event, a detailed discussion of the evolutionary biology of how complex multicellular organisms began to age is way beyond the scope of this post and beyond the scope of my knowledge of evolutionary biology, but one thing’s for sure. Aging is intrinsic to the vast majority of multicellular organisms, and telomerase is only made where and when it’s needed, such as in stem cells.
That’s not to say that there isn’t evidence that telomerase can’t prolong life expectancy. Andrews even cites some of it:
Would the concept apply to living organisms? In November 2008, scientists published a paper describing how they had created cloned mice from mouse cells containing the inserted telomerase gene, which continually produced the telomerase enzyme. These mice were shown to live 50% longer than cloned mice created from cells that didn’t contain the inserted telomerase gene.
It’s becoming increasingly clear that prevention of telomere shortening might be the best way to extend human lifespan beyond the theoretical 125-year maximum lifespan. How long this can extend the human lifespan is anyone’s guess, but living a healthy, youthful life to 250, 500, or even 1,000 years is not outside the realm of possibility. More research needs to be done to answer that question.
Maybe, but let’s just say I’m skeptical that telomerase alone can increase human lifespan that much if it could only increase a mouse’s lifespan by 50%. There’s so much more that goes into cellular aging than just telomerase, including increasing genomic instability through gradual accumulation of DNA damage, oxidative stress, and several other major mechanisms. That reminds me. One thing Andrews conveniently neglects to mention about the mouse model mentioned above is that telomerase was introduced into a mouse “engineered to be cancer resistant by means of enhanced expression of the tumor suppressors p53, p16, and p19ARF” in an “effort to dissociate the effects of telomerase on cancer and aging,” noting in the introduction:
Telomere shortening is an important barrier for the uncontrolled proliferation of tumor cells (Feldser and Greider, 2007, Blasco, 2005). In this context, it is not surprising that constitutive telomerase expression in several independent Tert-transgenic mouse models resulted in increased incidence of spontaneous tumors (González-Suárez et al., 2001, González-Suárez et al., 2002, Artandi et al., 2002, Canela et al., 2004). Therefore, in normal laboratory mice, the advantageous impact of telomerase on cancer cells obscures the potentially beneficial effects of telomerase in the context of normal cells and tissues; for this reason, we have resorted to cancer-resistant mice previously generated by us (Garcia-Cao et al., 2002, Matheu et al., 2004, Matheu et al., 2007). In particular, by transgenesis using large, nonmanipulated, genomic segments, we have generated mice carrying a single transgenic copy of p53 or a single transgenic copy of the locus encoding Arf and p16 (Garcia-Cao et al., 2002, Matheu et al., 2004). These three tumor suppressors are involved in protection against a large variety of cancers (Collado et al., 2007). The above-mentioned transgenic mice, which we call super-p53 (Sp53) or super-p16/Arf (Sp16/SArf), possess three gene doses of each of the indicated tumor suppressors instead of the normal diploid gene dose; this increase in tumor suppression activity is sufficient to significantly increase cancer resistance (Garcia-Cao et al., 2002, Matheu et al., 2004). Of relevance, single transgenic Sp53 or Sp16/SArf mice have a normal aging and life span (Garcia-Cao et al., 2002, Matheu et al., 2004), but the combination of both transgenes in doubly transgenic Sp53/Sp16/SArf mice results in delayed aging, probably because of the ability of these tumor suppressors to eliminate cellular damage and damaged cells (Matheu et al., 2007).
I also note that Anderson cites an earlier paper, one from 1999, to claim that driving excess telomerase production doesn’t in and of itself result in cancer, a nice sleight of hand, particularly his emphasizing that telomerase is not an oncogene (which appears to be true, given that it appears to be unable induce carcinogenesis by itself). However, that doesn’t mean that its expression doesn’t predispose to cancer, and a recent review notes that it is “still not established whether telomerase expression has any oncogenic characteristics or is simply required for the maintenance of sustained tumor growth (that is, whether it is permissive).” Again, even if telomerase is not oncogenic by itself, if activation of telomerase alone is not enough to cause cancer, that doesn’t mean it doesn’t contribute to cancer. If a cell with telomerase activity ramped up takes a “hit” that can result in cancer, telomerase activity plus that “hit” could result in cancer where the “hit” alone might not have. Even a 2012 mouse experiment (which, oddly enough, I don’t recall seeing in his booklet) that reported increasing mouse longevity without an increased incidence of cancer might well not be applicable to humans, given humans’ much longer lifespan, which provides much longer for cancer to develop. That’s why I find Dr. Anderson’s arguments at best disingenuous.
The last part of the booklet is puzzling, a real head-scratcher. Anderson goes on and on answering “objections”, such as: If we cure aging, then:
- Won’t the earth become overpopulated?
- Won’t Social Security be bankrupted?
- Isn’t curing aging unnatural or sacrilegious?
- Won’t future generations face challenges, such as long-lived dictators, that could have been avoided?
Oddly enough, he says little about the preclinical evidence for his treatment. He also even admits that some “scientists feel that curing cellular senescence is only a single piece of the aging puzzle, and that aging must be addressed on other fronts” and that telomerase “activation may or may not be the ‘magic bullet’ needed to achieve that end, but it’s a technology that’s well within reach, and any extension of lifespan could allow us to live long enough to see the next technology developed.” OK, then.
Interestingly, Anderson’s Cure Aging or Die Trying website appears no longer to exist, but the almighty Wayback Machine at Archive.org showed that it redirected to Sierra Sciences, which advertises something called TAM-818, billed as the “most potent telomerase inducer on the planet,” plus books with titles like Curing Aging and a YouTube video:
But what about the clinical trials? For that, we have to go to the Libella website and ClinicalTrials.gov.
Would you pay $1 million to sign up for a phase I trial?
When you visit the website for Libella Gene Therapeutics, LLC, you’re immediately greeted with this splashpage:
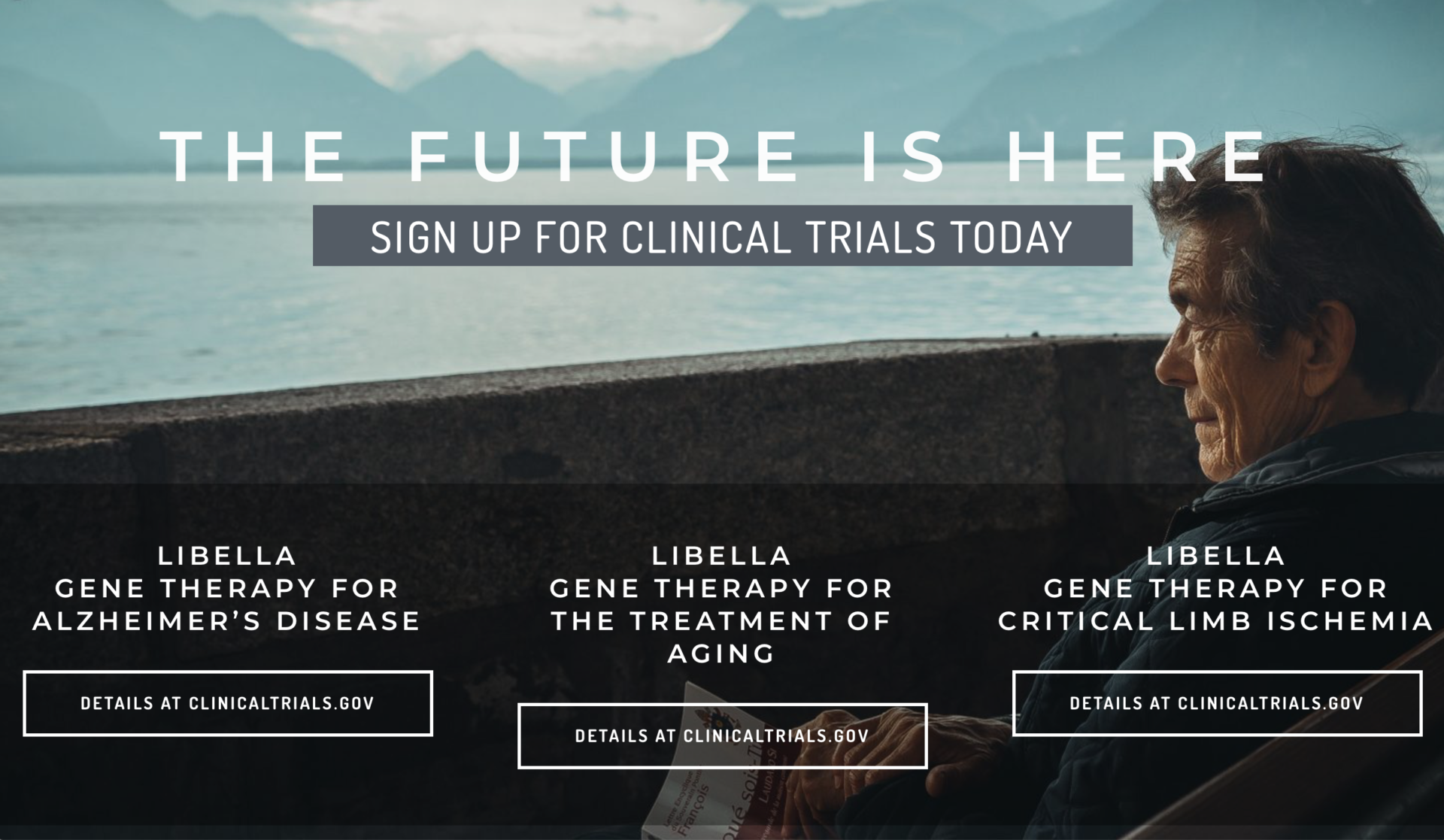
This splash page touts not just one, but three, clinical trials. They are:
- Evaluation of Safety and Tolerability of Libella Gene Therapy for Alzheimer’s Disease: AAV- hTERT (ClinicalTrials.gov identifier NCT04133454; first posted October 21, 2019)
- Evaluation of Safety and Tolerability of Libella Gene Therapy for the Treatment of Aging: AAV- hTERT (ClinicalTrials.gov identifier NCT04133649; first posted October 21, 2019)
- Evaluation of Safety and Tolerability of Libella Gene Therapy for Critical Limb Ischemia: AAV- hTERT (ClinicalTrials.gov identifier NCT04110964; first posted October 1, 2019)
The first thing that I noted was that these are all phase I trials, with an accrual goal of five patients each. That just means that they’re designed to assess safety, not efficacy, and even then, given the tiny numbers, only to detect really common adverse events. Remember, phase I trials are “first in human” trials whose main purpose is to assess safety, and indeed, the primary endpoints of each of the three trials are:
- For Alzheimer’s disease: Investigate the safety and tolerability of AAV-hTERT by IV and IT administration. (IT = intrathecal, into the cerebrospinal fluid)
- Antiaging study: Investigate the safety and tolerability of AAV-hTERT by intravenous (IV) administration.
- Ischemia study: Investigate the safety and tolerability of AAV-hTERT by intravenous (IV) administration.
Would you pay $1 million to be on a study that does nothing but evaluate the safety of the treatment and measure some telomerase-related biomarkers? A trial whose primary outcomes are basically tolerability and the incidence of serious adverse events? I sure wouldn’t, even if I were a billionaire!
And the secondary endpoints? Basically they’re pretty similar same for all three trials. Here are the endpoints for the antiaging trial:
- To determine changes from baseline in hTERT expression, telomerase activity, and telomere length in cells after treatment with AAV-hTERT.
- To determine changes from baseline in health and aging-related biomarkers after treatment with AAV-hTERT.
- To determine changes from baseline in the immune system after treatment with AAV-hTERT.
- To determine changes from baseline in physical function measures after treatment with AAV-hTERT
Which cells? Which immune system cells? Which biomarkers other than telomerase and telomere lengths? I really want to see the detailed protocol! I also would love to see the preclinical evidence. Libella features a list of research papers “related to our therapies.” I can’t help but note that most of them aren’t by Libella scientists and many of the papers co-authored by Andrews have little or nothing to do with telomerase. It’s the “pile of papers” method of justifying questionable research. I’ve seen it many times before. Dump out a list of papers, which might or might not report results that support and justify the work you want to do or, more commonly, are mixed in support and lack of support. Then don’t explain them or put them into context, and expect the reader just to be impressed by so much research, whether it supports your claims or not.
A highly unethical and dubious clinical trial
Reading Libella’s marketing hype, I couldn’t help but be strongly reminded of the marketing of stem cells of quack stem cell clinics, which make the same sorts of exaggerated or unjustified claims for clinical trials that are, like the Libella antiaging trial, no more than a phase I clinical trial that will almost certainly not benefit a single patient enrolled on it, while exposing them to risk. (Remember, the purpose of a phase I trial is to test for safety, not efficacy. I can’t repeat that enough.) Libella’s marketing materials keep referring to a 20 year old study in which human skin cells were grafted onto mice and telomerase expression made them much younger in phenotype, as if that were definitive preclinical evidence that their approach will work. It was infuriating to read. It is outrageous grift, in my not-so-humble opinion, to charge patients $1 million to sign up for a phase I trial of anything, much less an “antiaging” therapy with so thin a preclinical evidence base to justify bringing it to the clinic. I couldn’t determine for sure whether Libella is going to charge patients on the other two trials the same amount, or charge them at all, but the same criticisms apply to these trials, particularly the overhyped marketing. For example, the press release for the Alzheimer’s disease trial is titled “New Clinical Study May Be the World’s First Cure for Alzheimer’s Disease“. Yeah, right. Do we even know that telomerase has anything to do with Alzheimer’s disease other than that Alzheimer’s disease tends to be a neurodegenerative disease of aging? Sure, there is an association between shorter telomere length and accelerated telomere shortening in patients with Alzheimer’s disease, but is that just because of faster aging or does it actually have anything to do with Alzheimer’s?
Then there’s the clinic in Colombia. For all three trials, the principal investigator in Colombia is a man named Jorge Ulloa, MD at IPS Arcaslud SAS. A bit of Googling led me to conclude that this is probably the Dr. Jorge Ulloa Domingez who is running the trial for Libella. He’s a vascular surgeon who is the scientific director Fundación Vascular, a vascular clinic in Bogotà that specializes in venous diseases, and, as far as I could tell, appears not to possess any relevant training or experience to run a phase I clinical trial of gene therapy. His clinic, which appears to be his private practice clinic and has been in existence since 1980, is named after himself, El Instituto Vascular Jorge Ulloa Domínguez, or the Jorge Ulloa Domíngez Vascular Institute. The clinical trials themselves are listed as being performed at Clínica Arcasalud (IPS Arcasalud SAS) in Zipaquirá, Cundinamarca, near Bogotá. Its cover picture on its Facebook page sure doesn’t look like much:
Not being facile with Spanish, I couldn’t find out a heck of a lot more. Let’s just say, though, that what I’ve discovered doesn’t exactly fill me with confidence regarding the quality of science and medicine involved with what would even under ideal circumstances be a difficult trial.
So why did Libella decide to do the trial in Colombia? An anti-aging website Fight Aging! made this argument:
Neither Bioviva nor Libella took the standard regulatory path forward, opting for some combination of regulatory arbitrage and medical tourism to bring their therapies to patients. This sort of effort, carried out responsibly, is, I think, necessary and must spread if the present excesses of the FDA are to be reined in. The FDA sees its role as reducing risk to zero, at any and all cost, including the cost of slowing medical development to a crawl. Analyses have long shown that the cost in lives of this regulatory burden of slowed development far outweighs the benefits – but absent therapies are invisible and arouse no media outrage. Bureaucracies inevitably optimize to minimize visible problems. The only way to combat this issue effectively, given that working to change the system from within, and political advocacy to change the system from the outside, have been ongoing energetically for the past few decades, a time over which the financial burden imposed by the FDA has more than doubled, is to prove out a viable, responsible, cost-effective path to market outside the FDA system of regulation.
Libella Gene Therapeutics recently announced a patient paid trial to be held outside the US. Patient paid trials are unfairly excoriated by the research and regulatory establishment. As I have remarked upon in the past, they are an entirely legitimate approach to obtaining data. The chief objection is the lack of a control group in most such trials – but if we are only interested in large, reliable effect sizes, then the control group is the rest of the patient population, and that works just fine. In general, good therapies for aging, those that target relevant mechanisms in ways that will truly move the needle on life span, will indeed have large and reliable effects.
Yawn. No, the FDA does not cost lives through its caution. That’s a trope beloved by quacks, unscrupulous medical entrepreneurs, and FDA- and regulation-hating libertarians. If anything, the FDA is actually pretty fast at approvals when compared with other industrialized nations. Indeed, arguably, the FDA doesn’t require enough evidence for drug approval, and there’s been a problem with accelerated approval of drugs that later turn out not to be efficacious.
This interview with Libella’s President Dr. Jeff Mathis is also very telling:
Dr. Mathis’ justifications for sidestepping the US to do the trial of his gene therapy for Alzheimer’s disease in Colombia instead was unconvincing at best, and what about his claim that his gene therapy could be proven to work for Alzheimer’s disease within months? Well, here it is two years later, and that hasn’t happened.
In addition, as you can see above, Libella isn’t even the first company to go this route with a telomerase-based gene therapy. BioViva touts “advanced cell treatments” and “personalized therapy” based on your “unique genetics.”
Its website links almost exclusively to something called Integrated Health Systems, where its treatments are offered. The whole idea and platform are the same, delivery of telomerase to nerve tissues using AAV. Interestingly, I note that you can apply for treatment OR to be on the study. In the latter case, you’re greeted with:
You may qualify for a FREE $62,000 human study treatment.
Today 5.3 million people in the United States have Alzheimer’s Disease. Each one of them is sentenced to certain death if they have to wait for years of endless animal studies. That is why Max Life wants to go straight to the clinic for those who would otherwise have no hope.
Until now the FDA has approved no cure for Alzheimer’s disease. Our intention is to support research that demonstrates a successful treatment, and hopefully, a permanent cure within 12-18 months. Once proven, we hope to get FDA approval fast-tracked.
This is not only the humanitarian thing to do, but it will also save hundreds of billions of dollars annually — dollars that are currently being directed to patient care instead of a cure. Will you help make this clinical trial a reality? Will you help make this study a reality?
It all sounds very fishy and very scammy to me, even more so than the Libella study, as searches of ClinicalTrials.org for Bioviva or Integrated Health systems plus variants turned up no registered trials. Bioviva’s CEO, however, claims that her company’s product elongated her telomeres, after having “hopped on a plane to Colombia” in 2015 to receive “multiple injections of two experimental gene therapies her company had developed.” I can’t help but note that this report is from well over three years ago but that the company has not yet published its results or subjected them to peer review, as far as I can tell, although there is an update from 2018 claiming that her telomeres are longer still, at least in her white blood cells, which are all that were measured. There’s also the usual hype:
But aging is also preventable. We live in a golden age of technology, yet little is accessible and affordable to the general population, due to lack of knowledge, safety data and a general perception that aging cannot be helped. We have been taught that this is how life should end.
I refuse to subscribe to this complacency. I refuse to allow humanity not to benefit from the breakthrough scientific discoveries in the anti-aging field. I am not talking about cosmetics, but about whole body rejuvenation at cellular level. Humans are capable of living long healthy disease-free lives; we have anecdotal cases that prove this fact. I fight so that that these become the norm instead. I want my company to be a portal into a future of long healthy lifespans for all across the globe.
Then publish your case report and do science to obtain preclinical evidence to justify a clinical trial! I did a PubMed search for BioViva, and all I found were four papers, none of which had anything to do with telomerase! Also, demonstrate that managing to increase telomere length in white blood cells has any effect on immune function or aging whatsoever.
The bottom line is that I view Libella’s clinical trial to be profoundly unethical. I’d love to know which IRB they used to get regulatory approval in the US (required if they’re going to sign up patients in the US), because that’s an IRB that should not be evaluating clinical trials, given that it apparently approved at least one phase I clinical trial that charges patients $1 million to be treated in a trial that is not intended to benefit them and exposes them to risk of harm that is also being carried out in a country whose regulatory environment is—shall we say?—less than rigorous. (Again, it’s still unclear to me if the same charge is being required of patients enrolling in the other two trials.)
Let’s just put it this way. Libella’s marketing of its pay-to-pay antiaging clinical trial is so egregiously overblown that even enthusiastic advocates of “life extension” and “radical antiaging” treatments have problems with Libella’s marketing of it, with a man named Steve Hill even going so far as to call it “ridiculous” before writing:
This study will certainly cause controversy, especially given the huge price tag, which is likely what most media will focus on, but that isn’t the largest problem here. This has the potential to backfire very badly, and the resulting fallout could be harmful to credible researchers working in the field who are very careful about overpromising in the absence of results. While there is a need for marketing, good marketing can be done without resorting to unrestrained hype and nonsense. Ultimately, the success of this endeavor can only be determined with peer-reviewed data.
Hill also noted the lack of a control group. He didn’t, however, note that a phase I trial doesn’t have a control group and isn’t even designed to show efficacy. Maybe he didn’t know.
Meanwhile, back over at Fight Aging!, some of the commenters in the comment section after the article about the Libella trial were even more blunt, with frequent uses of the word “scam” and statements that it “sounds like a scam.” One even called it a “dangerous joke”, while another called it “snake oil.”
Meanwhile, someone named Dylan Mah wrote:
“These people” aren’t top thought leaders. They’re in the same basket as cryonicists; an albatross weighing down on the neck of legitimate researchers, siphon funding and damaging the reputation of actual, rigorously performed research that occupies the same sort of space in the public consciousness.
I can’t argue with Mr. Mah or any of the other commenters, who, I noted, are predisposed to support anti-aging research, other than that I find cryonics even more implausible than I find Libella’s gene therapy. In any event, Libella’s gene therapy trials sure sound to me like quackery no better than “clinical trials” run by the stem cell quacks I’ve discussed at length so many times before. Obviously, only the rich or those with access to a large line of credit will be able to afford a $1 million entry fee for Libella’s clinical trial, and one might be tempted to shrug one’s shoulders and ask: Who cares if a few super rich people waste a million bucks each on a trial that can’t help them? The problem is the precedent. The more companies get away with this sort of practice, the further they will push the envelope, and that will harm clinical trial efforts for treatments that aren’t as obviously dubious as the Libella trial.